Curriculum
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/Curriculum-image.jpg)
During the seven-year Neurologic Surgery Residency, you will receive advanced education in all aspects of neurosurgery, including both outpatient and hospital settings, with a full six months of dedicated intensive care unit (ICU) training. You will participate in the care and surgery of all neurosurgery patients as an integral member of the neurosurgical team.
Progressive responsibility and surgical experience under the direction of the neurosurgical faculty is assured throughout the residency. Each clinical rotation has specific competencies, goals, and learning objectives, in addition to the general departmental academic requirements.
Opportunities for enhanced training in a subspecialty area can be enfolded within the seven-year curriculum; present options include complex spine, peripheral nerve, and skull base.
Clinical training
As a resident, you are required to spend a minimum of 54 months of clinical neurosurgery training prior to graduation. A unique feature of the neurosurgery training at Mayo Clinic is our mentorship model, in which residents complete dedicated clinical rotations on the services of one to three faculty members for three-month periods of time. This provides for the development of a longitudinal relationship between you and staff, as well as an opportunity for true immersion in a particular practice model and complete continuity of care for the patients and families on those services.
Two years of dedicated research and career development time are afforded during senior residency. Supplemental clinical rotations, enfolded fellowships, and visiting electives may be arranged during this period. Additional provisions are allowed for residents desiring to expand their training by an additional year or longer, so as to obtain a doctorate in neurosciences through Mayo Clinic Graduate School of Biomedical Sciences.
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/curriculum/neuro-surg-mn-surgeon-1024X512-WF8098302_0002.jpg)
Typical rotation sequence
PGY-1
During your first year, you spend six months on the medical neurology services, including three months as junior resident in the neurosciences intensive care unit. Additionally, you spend one month neuro-otology, one month on plastics, one month on the chief resident service, and one month of neurophysiology.
By the end of this first year, the you will have a basic understanding of neurological disease and be competent to perform a neurological history and examination. You will have a strong knowledge base for evaluating and caring for the critically ill patient in an intensive care setting. In addition, you will have performed basic neurosurgical procedures including intracranial pressure (ICP) monitor placement, external ventricular drain, laminectomy exposures, and basic craniotomies.
This first year is expected to lay the foundation of knowledge and skills required for a superlative career in neurosurgery. On average, PGY-1 residents perform approximately 200 cases as first assistants.

PGY-2 and PGY-3
During these years, residents are assigned to quarterly rotations on the clinical neurosurgery services of the various consultants. The clinical assignment system is unique in that you work one-on-one with each staff neurosurgeon for three-month intervals before rotating. This allows the evolution of a strong teaching mentorship.
During these years, resident surgical skills significantly advance. It is expected that during this time, depending on your skill set, you will perform critical portions of each operation with the staff surgeon serving as an assistant and coach. It is also expected that you will better define your clinical interests and begin to formalize your career goals during the PGY-2 and PGY-3 years. On average, PGY-2 and PGY-3 residents perform approximately 400-500 cases per year as first assistants.
PGY-4
During the PGY-4 year, you will complete your trauma and pediatric rotations, as well as an elective at Mayo Clinic Rochester. You will spend five months at the University of Florida Health in Jacksonville, Florida for a trauma rotation learning complex cranial, complex spine, and cerebrovascular surgery. Additionally, four months are reserved for a dedicated pediatric neurosurgery rotation at Wolfson Children’s Hospital in Jacksonville, Florida, where you learn about complex pediatric neurosurgical pathologies. In addition, residents will also spend three months at Mayo Clinic in Rochester, Minnesota, for an elective neurosurgical rotation in the specialty of their choice. During this year, you take the American Board of Neurological Surgery written examination. A score at or above 75 percent is considered requisite for advancement to chief residency.
A formal, required curriculum of skull base, microvascular, and peripheral nerve techniques is simultaneously completed, both to facilitate anatomic study and to prepare residents for senior-level roles. Final planning decisions are made for upcoming career development. On average, PGY-4 residents perform approximately 500 cases per year as first assistants.
PGY-5 and PGY-6
Up to 24 months are allocated for career development, typically taken as a single block during the PGY-5 and PGY-6 time frame. Dedicated laboratory research, enfolded fellowships, visiting electives at Mayo Clinic's campuses in Florida and Arizona, and acquisition of advanced degrees are common academic pursuits during this time. But flexibility and adaptability to the needs of each individual resident's career are emphasized.
For residents who are pursuing a one- or two-year research block, applications for a Neurosurgery Research and Education Foundation (NREF) training grant and/or an NIH F32 training grant are highly encouraged. If basic research is chosen, a research plan should have been developed the preceding year with a mentor identified. Clinical research projects also may be chosen, and potentially pursued via the Clinician-Investigator Training Program or a master's degree.
The emphasis during the research year is toward the development of critical scientific methodology and production of meaningful contributions to basic science or clinical knowledge. For those pursuing additional clinical neurosurgery training, the goal is to develop advanced surgical training in a subspecialty area of interest.
Within these two years, both research and advanced clinical training can be combined. Furthermore, you are strongly encouraged to rotate to Mayo Clinic in Jacksonville, Florida, or Mayo Clinic in Phoenix/Scottsdale, Arizona, for advanced clinical training, notably in endovascular surgery, skull base and neuro-oncology surgery, complex adult spine surgery, or minimally invasive spine surgery.
PGY-7 (chief resident)
During the final 12 months of training, chief residents have responsibility for managing their own clinical service and operating room. This is unique among training programs.
Perhaps the greatest strength of our singular training program is that the Mayo Clinic chief residency allows senior trainees to function as junior faculty with the privileges of an autonomous starting operating room in which they are the primary surgeons. Chief resident cases are booked on an elective basis from their own active clinical practices. Further, you will manage all emergency neurosurgery cases and in-house consultations, providing for consultant-level decision-making and management across the full breadth of neurosurgery.
During this time as a chief resident, you will alternate emergency call, elective surgery, and outpatient consultation on a daily basis with a chief resident partner — a schedule akin to that of our full-time faculty. You are given the opportunity to rotate again for three to six months acting as a primary resident on senior faculty services to acquire additional expertise in areas of subspecialty training such as spine, cerebrovascular, endovascular, skull base, tumor, epilepsy, peripheral nerve, stereotactic surgery, or radiosurgery. On average, PGY-7 residents perform approximately 450-500 cases per year.
Call frequency
Call schedules vary by individual rotation. Mayo Clinic's Department of Neurologic Surgery follows the duty hour guidelines of the Accreditation Council for Graduate Medical Education (ACGME).
All residents share the in-house emergency call assignments equally during the time that they are assigned to clinical neurosurgery service, as well as during certain elective and basic science rotations. Therefore, the frequency of actually being in the hospital overnight to cover trauma and the emergency room is modest.
Residents on clinical neurosurgery services are expected to round on their service with the support of advanced practice providers, assist in those surgical cases, and direct specialty conferences. In-hospital night call covering emergencies occurs on average one out of every 14 days, as does "backup call," which is typically taken from home.
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/curriculum/neuro-surg-mn-microscope-1024X512-WF8098302_0020.jpg)
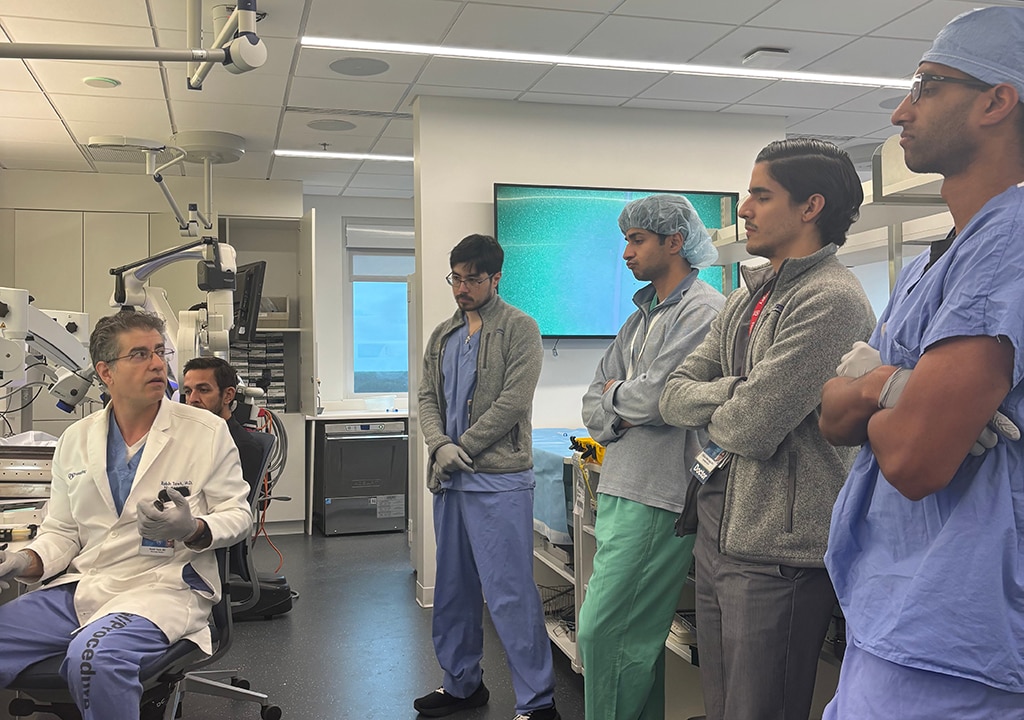
Didactic training
Didactic conferences are held on a daily basis for one hour, prior to the initiation of the day's operative calendar. Conferences are held in the neurosurgery department at Mayo Clinic and resident attendance is mandatory. This is a typical weekly schedule.
Neurosurgery Grand Rounds — Monday
There is a mock oral board case followed by a lecture typically given by neurosurgical colleagues from around the world. In 2019, there were 35 guest professors who discussed various issues from neurosurgical management to neuroscience research to economics of neurosurgery. All faculty and residents attend this conference.
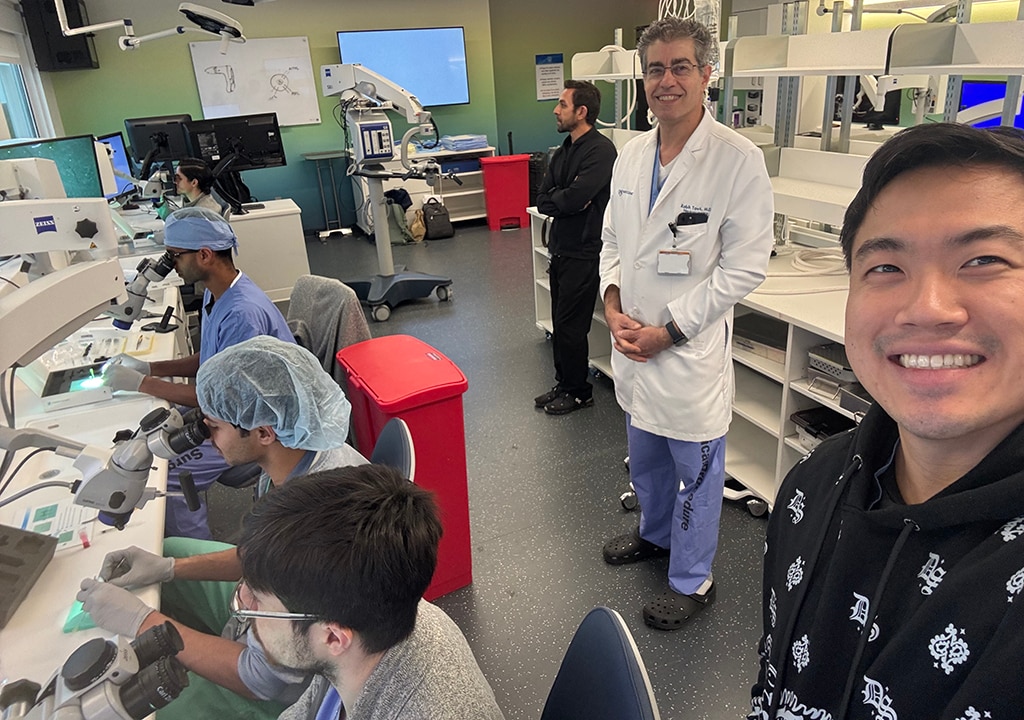
Resident Education Day — Monday (monthly)
The second Monday of every month is a faculty led case review, as resident led case discussion/question session in the morning. The afternoon is in the SIM lab, followed by a journal club.
Tumor Board — Thursday
Tumor Board is held on certain Thursdays.
Neuro-Oncology Conference — Friday
This is a multispecialty conference in which four interesting brain tumor cases are presented and discussed. The faculty from all the neuroscience specialties including neurology, medical oncology, neuropathology, and neuroradiology are in attendance. The format of this conference is standardized and educationally targeted, incorporating the case presentation, pertinent radiology, surgical approach, pathology, and adjunctive treatment with an open forum for discussion and analysis as appropriate.
Additional conferences
Multiple subspecialty conferences are held daily throughout Mayo Clinic, which are all open to neurosurgery residents. These include a neuroradiology conference, surgical epilepsy conference, pediatric neuro-oncology conference, and many others.
Case studies
The mandatory one-hour teaching conferences five days a week from 7-8 a.m. focus on both general and subspecialty neurosurgery. The subspecialty conferences include vascular, spine, epilepsy, neuro-oncology, and neuroradiology. These are held in conjunction with the appropriate medical and radiological services.
As a neurosurgery resident, you regularly contribute to the educational process, preparing case presentations, journal clubs, and didactic lectures.
Research training
As a neurosurgery resident, you are expected to engage in scholarly pursuits including clinical research projects and to participate in dedicated study and basic laboratory investigation under the direction of a research mentor during the elective research year. Members of the Department of Neurologic Surgery and other established investigators within Mayo Clinic's research departments serve as mentors and also assist you in developing your research proposal well in advance of the research year.
Financial support and call coverage is generally made available to residents whose research is accepted for presentation to national or regional neurosurgery meetings.
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/curriculum/neuro-surg-mn-surgeons-1024X512-WF8098302_0056.jpg)
Additional training opportunities
Clinician Investigator Training Program
The Clinician Investigator Training Program is available to residents who wish to prepare for an academic career involving a significant research component. This competitive program provides support for an additional one to two years of research outside of the usual scheduled resident rotations.
Upon completion, a certificate in clinical investigation for a master's degree in neurosurgery is awarded.
Clinical research training program
The Center for Clinical and Translational Science offers programs designed to train future investigators in clinical research through a curriculum focused on research methodology, complemented by mentor-based training in the research environment.
Options include a master's degree in clinical research, or a shorter program awarding a certificate in clinical research.
Doctoral degrees
There is a formalized pathway available to neurosurgery residents for obtaining a doctorate in molecular neuroscience, biomedical engineering, or molecular physiology, which requires a minimum of two to three years of study and research, culminating in a dissertation.
The in-residency doctoral program has been designed to maximize flexibility, allowing for an individualized curriculum, with appropriate oversight from an advisory and mentorship committee.
This program, offered in conjunction with Mayo Clinic Graduate School of Biomedical Sciences, should be strongly considered by neurosurgical residents interested in obtaining advanced basic science experience for a career in academic neurosurgery.
Career development
You are encouraged to meet formally and informally with the department chair, program director, and individual mentors on a regular basis to discuss career goals. The program director takes a sincere interest in tailoring your training program to career objectives and actively participates in job searches on behalf of all residents.
Mayo Clinic neurosurgery residents have been highly successful in competing for both academic and private practice positions, consistent with their individual goals.
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/curriculum/neuro-surg-mn-operating-1024X512-WF8098302_0006.jpg)
Teaching opportunities
Neurosurgery residents have the opportunity to teach Mayo Clinic Alix School of Medicine students and visiting student from other medical schools, through bedside instruction, formal didactic lectures, and voluntary participation in the anatomy curriculum.
Evaluation
Performance is carefully monitored throughout the course of the Neurologic Surgery Residency with an eye toward operative skill, clinical judgment, academic productivity, and career development. After each three-month clinical rotation, residents are evaluated formally by their supervising faculty.
Additionally, residents meet individually with the program director on a semiannual basis to review their performance and discuss career goals in detail to dynamically individualize their training program.
All residents sit for the American Board of Neurological Surgery written examination during their PGY-2 and PGY-3 years for self-assessment, and for credit during their PGY-4 year. A three-month neuropathology/neuroradiology rotation provides supplemental basic science education and opportunity for independent study prior to formal examination. You are expected to pass at a 75 percent or higher level before being qualified for the chief resident year.
As part of our regular examination of residents to monitor their progress and also help prepare for the future oral board examination, biweekly oral examinations in clinical neurosurgery and neurology are administered. The format is similar to that of the certifying oral examination given by the American Board of Neurological Surgery after completion of training. Feedback from the program director and director of resident education is provided.
An electronic case log program tracks all resident operative cases, with salient details auto-populated from the operative report and prepared for review and submission to ACGME case log. The case volume and mixture is carefully analyzed to ensure that you are obtaining in-depth expert training in all areas of neurosurgery. If areas of deficiency are identified, your rotations are adjusted accordingly to provide an appropriately balanced education.
/prod01/channel_2/media/mccms/content-assets/academics/residencies-and-fellowships/neurologic-surgery-residency-florida/curriculum/neuro-surg-mn-operation-1024X512-WF8098302_0040.jpg)